The State
of Disability
in Texas
A Texas Standard Special
Sometimes we say it with statistics: One quarter of Americans, many millions of Texans, live with a disability.
Sometimes we seek to tug at heartstrings, telling stories of overcoming obstacles – of the inspiration that we gain from learning about someone else's experience.
Some people live with disabilities their whole lives. Others find themselves navigating life differently after illness or injury.
Encompassing the wide array of these experiences in just one program would be impossible. But that's why we're treating this special as a kickoff of Texas Standard's yearlong commitment to featuring the voices of and covering the topics important to disabled Texans.
We want to hear from you. What stories should we tell? Which Texans should we celebrate?
Let us know what's on your mind:
‘We're slowly getting there’:
The legal landscape around disability rights in Texas
By Sarah Asch

Experts weigh in on where things stand after the 2023 legislative session.
Each legislative session, bills are filed that would make a difference for Texans with disabilities – and 2023 was no exception.
Lawmakers passed a measure requiring residential care facilities that receive Medicaid funds to do criminal background checks before hiring staff in an effort to protect those who live there, including individuals with developmental disabilities.
Other bills did not make it through the process, including one vetoed by Gov. Greg Abbott that would have established an accessible absentee voting system in the state.
The landscape around increasing opportunities and enhancing services for people with disabilities is complicated and ever-changing. To help us parse through the impact of recent legislation affecting Texans with disabilities, the Standard spoke with three people who work in the trenches of public policy affecting people with disabilities:
- Amy Litzinger, who directs the advocacy staff at Texas Parent to Parent, an organization that helps improve the lives of children living with disabilities.
- Chase Bearden, deputy executive director of the Coalition of Texans with Disabilities.
- Lauren Gerken, a policy analyst with the Texas Council for Developmental Disabilities.
From left, disability advocates Lauren Gerken, Amy Litzinger and Chase Bearden. Michael Minasi / Texas Standard
From left, disability advocates Lauren Gerken, Amy Litzinger and Chase Bearden. Michael Minasi / Texas Standard
This Q&A has been edited for length and clarity:
Texas Standard: Let's start with a very broad question. Over the last decade or so, the legal landscape for Texans has changed when it comes to disability. Have things generally been getting better or worse for people with disabilities in the state? Chase, let's start with you.
Chase Bearden: I think we've had an uptick of trying to improve different areas, and we're slowly getting there. But every legislative session, or as technology changes, we're facing new barriers in the workplace and in the community.
So I think it's an ever-changing landscape. But I think we're seeing more people in the disability community doing more and being able to do more based on a lot of the protections and services that we've put out there over the years.
Lauren, how do you feel about that?
Lauren Gerken: Yeah, I agree. I'm a big believer that the arc of progress is slow but moving. We've seen some improvement in terms of guardianship policy in Texas for people with disabilities.
We've seen the increase in general awareness of disability issues in policy and a greater understanding of how people with disabilities are affected and that they are an important part of the fabric of our society, and that we have to really focus on improving inclusion. And moving forward, we are not going away, so we have to integrate us better.
‘I'm a big believer that the arc of progress is slow but moving,’ says Lauren Gerken, a policy analyst with the Texas Council for Developmental Disabilities. Michael Minasi / Texas Standard
‘I'm a big believer that the arc of progress is slow but moving,’ says Lauren Gerken, a policy analyst with the Texas Council for Developmental Disabilities. Michael Minasi / Texas Standard
Amy, what's your take on that? Do you feel like things are improving generally?
Amy Litzinger: From a policy perspective, yeah, we are making progress. But not only are we all policy people in the disability arena, we're all people with disabilities, so sometimes it feels like, yeah, the policy’s improving, but boots on the ground, I actually have to live with my disability and the consequences of the policy that may not change as fast as I need them to day-to-day.
So yeah, things are improving, but we need to make sure that they're not just improving on a philosophical level – that we actually see, what does this look like in people's daily life? Which I think we're not seeing enough of.
I wonder, as somebody who's both an advocate and a person with a disability, do you feel like those dual identities make it easier for you to be an advocate and to explain to people who might not understand the sort of details of the public policy you're working on?
AL: It helps from the policy side because I can use my own life as an example, but it doesn't help from a person with the disability side sometimes because I feel like I know too much for my own good, and I know exactly why I'm not getting the support they need. And it feels like it's my job to fix it by myself.
Let's talk about the legislative session in 2023. Are there any particular big wins or frustrations that you had this session? Amy, let's start with you.
AL: Education had several big losses. With the idea of vouchers, we're worried that special ed funding is going to be taken away to fund the vouchers so that there's less money for school districts to work with in their special education budget.
And anecdotally from our members, we've heard that if they go to a charter school or a nonpublic school, it only works for a while because the federal Individuals with Disabilities Education Act is not followed. And then a couple of months later, they have to go back into the public schools anyway. But the public school has already lost the funding that was used in the vouchers.
‘Sometimes it feels like, yeah, the policy’s improving, but boots on the ground, I actually have to live with my disability and the consequences of the policy that may not change as fast as I need them to day-to-day,’ says Amy Litzinger, who directs the advocacy staff at Texas Parent to Parent. Michael Minasi / Texas Standard
‘Sometimes it feels like, yeah, the policy’s improving, but boots on the ground, I actually have to live with my disability and the consequences of the policy that may not change as fast as I need them to day-to-day,’ says Amy Litzinger, who directs the advocacy staff at Texas Parent to Parent. Michael Minasi / Texas Standard
Chase, how about you? Any victories during the legislative session this time, or frustrations that you experienced?
CB: I would throw out there as both a victory and a real frustration: A lot of the work we did was around elections. I think passing House Bill 3159, which would have made accessible mail-in ballots for people with disabilities – especially those who are visually impaired or have upper body extremity loss to be able to cast a mail in ballot independently – has taken a lot of years and a lot of sessions to really explain to people and work through.
And the reason I say it was a win is that we were able to get bipartisan support across the board. I believe there were only five legislators who voted against it. When do you get that in a voting bill? And it was something that we really worked hard with the Secretary of State's Office, with all of the legislators.
The disappointment came on the last day of vetoes when the bill was vetoed by Gov. Abbott and no one was really given a heads-up. And our hope is that we can continue working with the governor. He said he believed it was a good bill and that we just need to make some adjustments and that it will come up in a special session.
At the end of the day, it was a big win just to get the acknowledgement from all the legislators that it was the right thing to do – and from the Secretary of State's Office.
Lauren, what's your perspective on the legislative session?
LG: So, we also saw some wins and some setbacks – I think that is pretty normal in a legislative session. We have been looking at the issue of parents of children with disabilities who are unable to find a daycare facility in their area that will accept children with disabilities. Some facilities won’t accept children with disabilities as a blanket statement without doing any analysis of what accommodations that child may or may not need.
We had a bill this session – and last session and the session before that – that would really address that issue by ensuring that licensed childcare facilities in Texas understand that they're not permitted to discriminate based on disability.
That bill in the past had not made it out of the committee that it was in. And this session it did make it through the committee, and it made it to the House floor, and it got voted through the House. The legislation as it's currently written will get filed that way next session, and we’ll already be set up in a better position than we were this session.
Texas Standard's Shelly Brisbin leads a roundtable discussion with disability advocates Amy Litzinger, Chase Bearden and Lauren Gerken in the Texas Standard studio. Michael Minasi / Texas Standard
Texas Standard's Shelly Brisbin leads a roundtable discussion with disability advocates Amy Litzinger, Chase Bearden and Lauren Gerken in the Texas Standard studio. Michael Minasi / Texas Standard
Looking forward, I'm wondering, what are the big policy areas or priorities that you are focusing on? Let's start with you, Amy.
AL: I am really worried about this attendant wage situation, because it used to be that this was a competitive wage, but we haven't had a cost-of-living increase for as long as I've had services, and I've had this half my life.
So instead of this being a good entry-level job, we're now $5 lower than most fast-food restaurants. So that's a big issue for me as someone who accesses attendants. But the other thing is the waiting list is almost a lifetime long at this point.
But we need to do both of them together, because if we reduce the waiting list and then they can't fill any of the positions, we have a problem. But if we increase the wages and we still have 160,000 people who can't even access anything, that's a problem, too.
Chase, what about you? What are your priorities for the future?
CB: Attendant care is one of the key ones that all of our members always talk about, and it's probably one of the biggest issues. We'll continue working on elections and making sure we remove barriers and make sure there aren't new ones being put in place.
And then just working from there on any other area where access can be improved so that people with disabilities can just live as full of a life as they want to live.
Lauren, what are your priorities going forward?
LG: We all have many. One of ours is looking at Medicaid income limits. So when people have Medicaid or are on a Medicaid waiver, they have an income limit that is adjacent to supplemental security income. And that is a pretty low number where if somebody who has Medicaid services wants to go get employed, they begin to earn more than their income limit.
And we have seen instances where a person receiving Medicaid services – which often is crucial to getting up and getting out of bed and getting to work in the morning – ends up earning a little more than their income limit and they lose their Medicaid, and it sets them back because they often lose the services that are helping them maintain their employment.
So we are really interested in exploring what the options are for navigating that income limit – or better yet, increasing that income limit – to respect the fact that people want to and can have competitive and paid employment.
Get more news from around the state:
Baylor program breaks new ground in autism treatment by focusing on sibling relationships
By Glorie G. Martinez
Parents often act as caregivers for their children. But when it comes to those who require lifelong assistance, a big question emerges: Who will take on this role in the later years?
Over 3.5 million Texans have at least one disability, according to data from the 2021 American Community Survey. Under that umbrella are people leading diverse lives: Some live independently, while others may require support for daily life tasks. For many, family members and caregivers play a pivotal role.
Parents often step in as caregivers for their children. But when it comes to those who require lifelong assistance, a big question emerges: Who will take on this role in the later years?
At Baylor University in Waco, an innovative program aims to offer an answer by focusing on sibling relationships.
“Siblings sometimes aren't noticed as much as other family members, so parent training is very important,” said Jessica Akers, an assistant professor of educational psychology at Baylor. “But we often leave behind siblings who are going to be lifelong comrades of their sibling with autism.”
Akers, who has personal experience with siblings on the autism spectrum, this year launched the Sibling SUCCESS program, which aims to strengthen sibling bonds and teach essential caretaking skills.
David, Jessica Akers' brother, helped inspire the Sibling SUCCESS program, which aims to strengthen sibling bonds and teach essential caretaking skills.
David, Jessica Akers' brother, helped inspire the Sibling SUCCESS program, which aims to strengthen sibling bonds and teach essential caretaking skills.
“Siblings have a really unique perspective on their sibling with autism,” Akers said. “Like, their parents will come and ask them, ‘like, what's he saying right now?’ And they know because they have a much closer bond in that way.”
Drawing from her own experiences, Akers believes that experiences shared between siblings – like the special version of tag she played with her own autistic brother – help create a unique connection that can be harnessed effectively to improve behavioral treatment.
“Often, siblings get included once they have to be included – so, once a parent passes away and then they're the only one there,” Akers said. “A lot of siblings feel like it’s something that gets dumped in their lap, and they have no idea how to navigate the service providers or any of the systems.”
Under current treatment models, some siblings feel excluded from caregiving. Like Akers, Baylor accounting grad student Jade Van Wyk grew up with a sibling with autism. She's now the president of a student organization called the Bears Autism Spectrum Society.
“When someone would come to our house to do therapy or just help her, it was like, ‘okay, now you have to go to another room and like, I need to work with your sister,’” she said. For Van Wyk, who often felt like she was the only one who understood her sister, the exclusion didn’t make sense.
A main focus of Sibling SUCCESS is to involve siblings in caretaking conversations sooner so that they understand their sibling’s condition and are equipped with essential skills.
The program offers three tiers of training, ranging from one-day workshops to extended programs. The focus is on children with autism ages 5 to 18, as well as their siblings. But the program isn’t all about caregiving logistics – it also delves into creating healthier sibling relationships.
“At the beginning, we interview the siblings and ask them things like, ‘what is your brother really good at that no one knows about?’ Or ‘what's something you wish you could do with him, but you can't right now?’” Akers said. “We write goals that are specific to the siblings – playing together, maybe requesting things from their sibling instead of grabbing things.”
Akers' program also creates a space for non-autistic siblings to connect with peers who share similar life experiences. This kind of peer support provides a sense of understanding and validation that can seem all too rare.
“There might be people that know about autism or that have had experiences with people on the spectrum. But it's always different to meet a sibling who was raised alongside someone with autism,” Van Wyk said. “It is just a totally different experience. You don't feel weird mentioning things, or you don't feel like someone is going to pity you or like, think you had a weird life.”
Van Wyk knows that there's no one-size-fits-all approach for families with autism – but she thinks Akers is on the right track by acknowledging the importance of sibling bonds.
“What the Sibling SUCCESS program does, like, I think it's really beneficial to have that sibling's input,” Van Wyk said. “Not to put all the burden on the sibling and not to make them a teacher. But as long as they're willing, it would still be helpful to teach them how to navigate that.”
Over the next three years, the Sibling SUCCESS team hopes to work with 125 families across Central Texas. For more information, email [email protected].
Lack of transportation options limits opportunities for people with disabilities
By Alexandra Hart

Those living in rural areas have an especially difficult time accessing transit.
In car-loving Texas, driving from point A to point B is the default way of getting around for most people. But that isn’t an option for some, including Texans with disabilities.
Barbara Spear, a retired schoolteacher living in a small town in South Texas, is one of them. She’s lived in both cities and rural areas, and she said that each presents its own challenges when it comes to getting around.
Her town doesn’t have a bus system, or Uber or Lyft, so options are limited. There’s a county-run call-in ride service, but it requires scheduling in advance. It also can get expensive quickly and isn’t a sustainable option for regular use, she said.
“If you cross more than one county line and you cross more than one city limit line, then there's an extra charge for all of that, and the service becomes unaffordable for a group of people who are vastly under hired,” Spear said. “And many times our income is much lower than the training and the skills that we have, which comes from decades of job discrimination, which still exists. So our income has a direct impact, especially if we live in rural areas, on where we can go.”
A report from the University of Montana found that some 6 million Americans with disabilities struggle to meet their transportation needs – especially in rural areas. Lack of access to transportation means people are less likely to leave home for work, socialization and enjoyment, leading to worse financial and emotional well-being outcomes.
Even in areas with public transit and paratransit options, navigating the city with a disability can be a challenge. Virginia Dize, director of transportation for USAging, said that reliability of transit services can be a barrier for people with disabilities, especially those who need to get to appointments or access other services.
“There may be good transportation available Monday through Friday during the day if you need to go back and forth to work. So the schedule is really great,” Dize said. “But if you have a mid-afternoon doctor's appointment, can you get home using the service that's available? And frequently there's no service on weekends. And we know that a lot of people, particularly dialysis patients, a lot of them get dialysis on Saturday.”
Plus, poorly maintained or nonexistent sidewalks can make bus stops inaccessible to wheelchair users, and uncovered bus stops or bus stops without seating can make waiting for transit unsafe for people with chronic illness.
A man sits waiting at an uncovered Austin bus stop amid sweltering Texas heat. Patricia Lim / KUT
A man sits waiting at an uncovered Austin bus stop amid sweltering Texas heat. Patricia Lim / KUT
Another barrier to access, even in places well-served by transit options, is lack of awareness, Dize said, especially among those who are newly disabled.
“A lot of older adults with disabilities may not apply [for paratransit] because they don't necessarily recognize themselves as having a disability,” Dize said. “Also, a lot of people just simply don't know about the service, especially if they previously drove a car. So paratransit is a very important service and it serves a lot of people, but a lot of people don't take advantage of it.”
One solution that’s gaining popularity in underserved areas is volunteer ride-sharing services. This can be a more convenient and comfortable option, according to Dize, but still has its limits.
“We also have found when we have a survey on older adults and people with disabilities that the preferred way of travel for many people is in the car individually,” Dize said. “And of course, those services are not universally available, but there are lots of places where they offer volunteer transportation that can offer that service. But a lot of volunteer transportation does not serve people in wheelchairs.”
Of course, creating and improving services like these and others requires funding. Dize said that several government funding programs are available for communities, including something called Section 5310 from the Federal Transit Administration. Those funds can be used for things like purchasing vehicles for programs and hiring mobility managers to coordinate transit in underserved areas.
More affordable options, Spear said, would go a long way in helping make life easier for people like her.
“I'm not saying that we shouldn't have to budget our trips just like [non-disabled people] do. I'm not saying that at all,” she said. “It's just that we really don't have the option of being able to go where we need to go as often as we would like to. But, you know, that's life; you get used to that.”
Resources:
- Call 211 or visit 211texas.org to get connected to local transportation offices
- The Administration for Community Living’s Disability Information and Access Line can be reached by call, text or video phone at 888-677-1199, or by visiting acl.gov/DIAL
- The ACL also has an eldercare locator at eldercare.acl.gov or by calling 1-800-677-1116
'We can still do great things that other people can do,' says young novelist
By Molly-Jo Tilton
Holly Foster, a 10-year-old born with congenital muscular dystrophy, has written her debut novel, ‘Camp Misty Woods.’
For 10-year-old Holly Foster, a love of reading naturally led to writing her own book.
“When I was younger, I read – well, I still read a lot of books – but I read a lot of books, and eventually I decided, well, I'm doing my own book,” she said.
The San Antonian’s debut novel, “Camp Misty Woods,” clocks in at about 35,000 words long and tells the story of four kids who go to a summer camp with horses – and find some magical adventure along the way. In the book, Holly writes:
My heart pounded as I looked at the trees to the left and right of us. I shuddered as we passed an old tree. It was bent over in a funny way that made it look like a crooked old man begging for help with his falling apart arms, and his mouth was all zig-zaggy, looking suspiciously miserable ... He probably had some kind of disease that he really just wanted to get other people sick with.
That's ridiculous. More like it got struck by lightning so it looks like a screaming mouth and a crooked back, I thought, but really it still looked creepy when I looked at it.
“It makes me feel happy because I had always wanted to write a book, and then everybody liked it,” said Holly, who had a book signing at school.
Holly said that living with congenital muscular dystrophy means she can’t walk like other kids, so she’s found other things to do – like drawing, reading and writing.
"When I'm reading, I feel like I get to be in another world for a little bit,” she said. “I want people to know that even though we can't do, like, some things other people can do, we’re still very capable, and we can still do great things that other people can do.”
10-year-old Holly Foster, of San Antonio, recently published her debut novel "Camp Misty Woods." Molly-Jo Tilton / Texas Standard
10-year-old Holly Foster, of San Antonio, recently published her debut novel "Camp Misty Woods." Molly-Jo Tilton / Texas Standard
Holly Foster enjoys a treat at an event with her brother. Courtesy photo
Holly Foster enjoys a treat at an event with her brother. Courtesy photo
Audio description for dance brings movement, emotion to visually impaired audiences
By Michael Marks

The practice is a verbal translation of visual information.
There’s no dialogue for about the first eight minutes of the movie “E.T. the Extra-Terrestrial.” John Williams’ score plays as the movie opens with a spaceship, a chase through the woods, and the title character eventually getting left behind on Earth.
“The first actual dialogue is the kids sitting around the table in the kitchen of their house. So a person who is blind has to spend the rest of the movie trying to figure out what is the purpose of the movie,” said Celia Hughes, executive director of Art Spark Texas, which produces art programs for underserved communities around the state.
Audio description can fill in the gaps, though. Audio describers relate key visual information, so visually impaired members of an audience can follow what’s going on in a show, movie or any other medium that relies on an ability to see. Hughes has been doing it for years.
“Through audio description, you describe that whole opening sequence [of E.T.],” she said. “So a person who’s blind has an equitable experience – they know exactly what’s happening when the dialogue begins in the kitchen.”
Audio description has been around for about 40 years. For a long time, describers were taught to keep a neutral tone: no opinions, no editorializing, just the facts.
But that is starting to change – especially in audio description for dance.
“One of the reasons that’s happening is because we have blind dancers who are now involved in audio description,” Hughes said. “They’re like ‘No, this hasn’t been a good experience for me; let’s make it better.’ From that is coming this whole new notion of what is the emotion of the story.”
Kayla Hamilton, a dancer and educator, is one of the people pushing this transition. Hamilton, who’s originally from Texarkana and now lives in the Bronx, is visually impaired herself and develops dances and description in tandem.
“I want to know what’s happening with, like, specific body parts, basically. I care about the races of the people, the body types of the people,” she said. “Anything that can give me political information I want to know about, because whether we acknowledge it or not, all those things impact what we’re experiencing.”
In a piece called Unearthing the Dark, Hamilton performed the same movements over and over again with different descriptions playing for the audience. Some were clinical, almost robotic. Others had nearly no description of movement at all – just emotion. For her, audio description is malleable.
“Maybe in this one particular section, it’s super important to know what the body is doing. Another place, I can give a little more context or feeling,” she said. “And I also think feeling can come through in the way the description’s being delivered, using like tone.”
Some dances are more straightforward to describe than others. A modern, abstract piece can present challenges that something with a clear story may not. A big ensemble number is more complicated than a solo.
For any performance, though, getting as much practice as possible is always preferable, says Allison Tignor, an audio describer from Houston.
“The more that I’ve previewed it the easier it is, because I know what’s coming,” she said. “But if I have to describe it the first time, that’s the first time I’m saying any of these things, and it’s coming right off the top of my head. If I do it a second time or a third time, like, it’d get easier every time.”
Tignor recently described “Peter & Wendy,” a show based on “Peter Pan” put on by Houston’s Open Dance Project.
The performance was at Miller Outdoor Theatre, a covered stage at a park near the center of town. The stage looks out on a big open space with seats and a lawn. Tignor sits in a tiny soundproof box behind all the seats, with an air conditioner blasting to keep the evening humidity away.
During the show, Tignor talks into a microphone that broadcasts to headsets provided to visually impaired folks before the performance. Someone else coordinates that, because if there’s a technical problem, Tignor can’t stop describing in the middle of a show to deal with it.
Before the show starts, audio describers generally read pre-show notes that give the audience a preview of the characters, their costumes, the set and other visual details.
Once it begins, the music comes through a scratchy little speaker in the soundproof room. Except for entrances and exits, Tignor doesn’t use a lot of notes. She has to be totally locked into what’s happening on stage.
“I’m having to be engaged in the same way that I would be in a conversation. I might only be talking, but I’m waiting for them to give me information,” she said. “And then I’m talking, and I take information, and I’m talking, and I take information."
'Often the disabilities are invisible' for long COVID patients experiencing a range of symptoms
By Laura Rice
Seventeen percent of Texas adults have experienced or are currently experiencing long COVID, according to a recent CDC survey.
Some disabilities are obvious to other people. Others are hidden. The Invisible Disabilities Association says hidden disabilities include fatigue, pain or cognitive dysfunction, among many others.
These are some of the same symptoms people experience with long COVID. And indeed, the federal government says long COVID qualifies as a disability under the Americans with Disabilities Act.
A recent survey from the Centers for Disease Control and Prevention shows that 17% of Texas adults have experienced or currently are experiencing long COVID, and about 5% said it has limited their activities.
For more on our understanding of long COVID and how it's affecting Texans, we turned to two people leading the field here in the state:
- Dr. Esther Melamed, an assistant professor in the Department of Neurology at the UT Austin Dell Medical School and research director at UT Health's post-COVID-19 program.
- Dr. Monica Verduzco-Gutierrez, professor and chair in the Department of Physical and Medical Rehabilitation at UT Health San Antonio and the developer of a post-COVID-19 recovery clinic there.
This transcript has been edited lightly for clarity:
Texas Standard: Dr. Melamed, what is your understanding right now about how common it is to develop long COVID symptoms?
Esther Melamed: That's a great question, and it's a little bit not understood completely. However, studies are demonstrating that at least 10% to 30% of individuals who had acute COVID go on to develop long COVID. Some studies actually cite as high as 60%. And people have developed different types of symptoms of long COVID that may qualify them for that diagnosis
Back Row - Left to right: Kat Motovilov, Cole Maguire, Matthew Petershack, Sam Bazzi, Adriana Souto Periera Nu; Front Row - left to right: Akshara Ramasamy, Dr. Esther Melamed, Netta Blinchevsky. Emily Kinsolving / UT Health Austin
Back Row - Left to right: Kat Motovilov, Cole Maguire, Matthew Petershack, Sam Bazzi, Adriana Souto Periera Nu; Front Row - left to right: Akshara Ramasamy, Dr. Esther Melamed, Netta Blinchevsky. Emily Kinsolving / UT Health Austin
I think that's really a surprisingly high number. Does it strike you that way as well?
EM: There are so many different symptoms that patients are experiencing. And the percentage that has been cited really includes people who develop anywhere from one to over 30 different symptoms. And that probably, depending on the study, will make the number of patients appear larger or lower, depending on how many symptoms are encompassed in that definition.
And I should also note that the definition of long COVID is really evolving at this time. And as we learn more about this new and complex disease, hopefully we will get to a better prevalence – the actual prevalence – of the disease.
Monica Verduzco-Gutierrez: I'm going to also add something to this about the number of people who have long COVID: These are the numbers that we have at this moment and with people maybe only having one infection. What we don't know yet – and what we are very concerned about – is reinfections.
You know, COVID is around – it's endemic; it seems like it's going to have little surges every few months, every year. And what's going to happen when someone's been infected three, four or five time,s and how the rates of long COVID will go up with that?
Can you also talk a little bit about the kinds of symptoms that you've seen in your clinic for long COVID patients?
MV: So there's something that I say when I talk about the symptoms and the patients that I see: If you've seen one patient with long COVID, you've seen one patient with long COVID. And that means that there can be so many symptoms. There's one study where they looked at over 200 symptoms that patients with long COVID had, who are having lingering effects after the infection.
So definitely, you know, one major thing is fatigue – but not just regular fatigue, fatigue that's also called post exertional malaise. So that means someone might be doing the activity that they were used to doing before and seems very simple, but after trying that activity, they have a crash and maybe they can't get out of bed, or they're just knocked out for two days.
Along with that, patients can also have symptoms of POTS, which are headaches, palpitations, heart rate going up when they're standing or doing activities. We know that patients can have pains in any parts of their body. We know that they can develop diseases afterwards as well. Patients can have migraines and severe dizziness. It's just, really, you name it, COVID can make it worse.
Dr. Melamed, can you talk about what we know currently about how COVID-19 affects the brain in long-term COVID cases?
EM: We're finding that among the multiple symptoms that Dr. Gutierrez mentioned, neurological symptoms are some of the most common ones that we see. And patients present with difficulty with attention, concentration and memory, which collectively has been termed by patients as “brain fog.”
In addition, patients develop neuropathies where they have pain in different parts of their bodies. Many of these patients go on to have documented small fiber neuropathies. These are types of neuropathies that affect the tiniest of the nerves in the extremities, in the arms and legs.
Patients also develop different types of dysautonomias where their heart will start to palpitate all of a sudden and they may have dizziness. And that is due to the failure of the autonomic nervous system.
And as a result of these neurological symptoms, a lot of patients feel extremely disabled. And that is one of the leading causes of why people say they may no longer be able to work.
Dr. Verduzco-Gutierrez, how have some of your patients who have long COVID been accessing some of the resources and benefits available via the ADA?
MV: It is nice that the ADA does recognize long COVID as a disability. So that means that as a physician, I can write accommodations for a patient who may have to work but have accommodations.
So that means I will try to do as much as possible to make a patient who has long COVID successful in the workplace. That might be asking for telework, if someone has that type of job that allows for telework; we know that not everyone always has such luxuries in what they do. I may ask for someone to have a gradual return-to-work program as they see how much they can tolerate – so maybe they just start at four hours a day instead of going full eight hours a day.
And so these are the types of accommodations. But again, that would mean that someone who has long COVID would be able to access a physician who'd be willing to write for accommodations for their workplace to follow.
Julia Reihs / KUT
Julia Reihs / KUT
Dr. Melamed, have you also seen your patients use ADA resources, and has it been a struggle for them? Have folks had difficulty redefining themselves as somebody with a disability?
EM: Yeah, it's a really important question. For long COVID patients, often the disabilities are invisible, where they're having the extreme fatigue, where they're not able to get out of bed, or if they do an activity, then for the next couple of days they're fatigued. They're having all of the neurological symptoms of brain fog and pain and headaches. And a lot of these are invisible.
And as a result, it becomes very challenging for patients to be able to explain to their family members and to people at work that they're actually not feeling well when others can't visibly see that they're not able to do the things that they say that they can't do.
And that does really change people's perspective on who they are as individuals. How are they viewed by their families, by their coworkers, by their friends? I've seen people start to really redefine themselves and what's meaningful for them and who is meaningful in their lives and who is there to continue to support them with this invisible disability.
MV: The other thing we see is stigma. There's been even research showing that these patients really feel that they've had high rates of stigma and discrimination against them because of, again, as you've described, their invisible disability.
Dr. Verduzco-Gutierrez, you also have experienced long COVID yourself. You're an expert in the field, but this is something that's personal for you. Can you talk about that experience?
MV: I had COVID over a year ago. It was a very, very mild case. I was vaccinated and didn't even feel that bad when I was acutely ill. And about two weeks afterwards is really when I had the symptoms come on and did have some of those palpitations, dizziness, very severe fatigue; exercise intolerance happened for a long time as well. And migraines were very, very bad.
And so these are things that I had to learn to control and had to manage my own symptoms without trying to be my own doctor and try to get help from other physicians who didn't know as much as I did about the field. I'm feeling much, much better now, and I have the tools to control my symptoms and to make myself feel better.
And I was able, thankfully, to work the whole time. And some patients are not at all that lucky. But I definitely don't want to get COVID again. I don't want to get sick again because I don't want to go through it again or make it worse.
Dr. Melamed, as we see new strains of COVID-19 coming out, should we expect that more Texans will be getting long COVID?
EM: It is something that we're going to continue to have to research and to understand better how the different strains affect the rates and the severity of long COVID. We've certainly seen evidence that people who had developed long COVID with the earlier strains of SARS-CoV-2, with alpha and delta, developed more severe long COVID symptoms that that have been lasting longer.
However, people continued to develop long COVID with omicron, which was presumed to be a milder strain of SARS-CoV-2. And as Dr. Gutierrez mentioned, we do see evidence that reinfections contribute to higher rates of long COVID, and the continued mutations of the virus may do so as well.
So, at this point in time, it does seem that this has become an endemic virus that will continue on, and reinfections may contribute to the worsening of the underlying symptoms that patients experienced or contribute to new cases.
And I should just mention that in terms of worsening of symptoms, we've seen a lot of patients in the post-COVID clinic who come in and say, “I have felt better. It's been about a year. I'm now doing a lot more activities. I feel so much better.” And then they get reinfected, and their symptoms come right back.
And so I think we're going to continue to learn about what the new strains bring on in terms of long COVID.
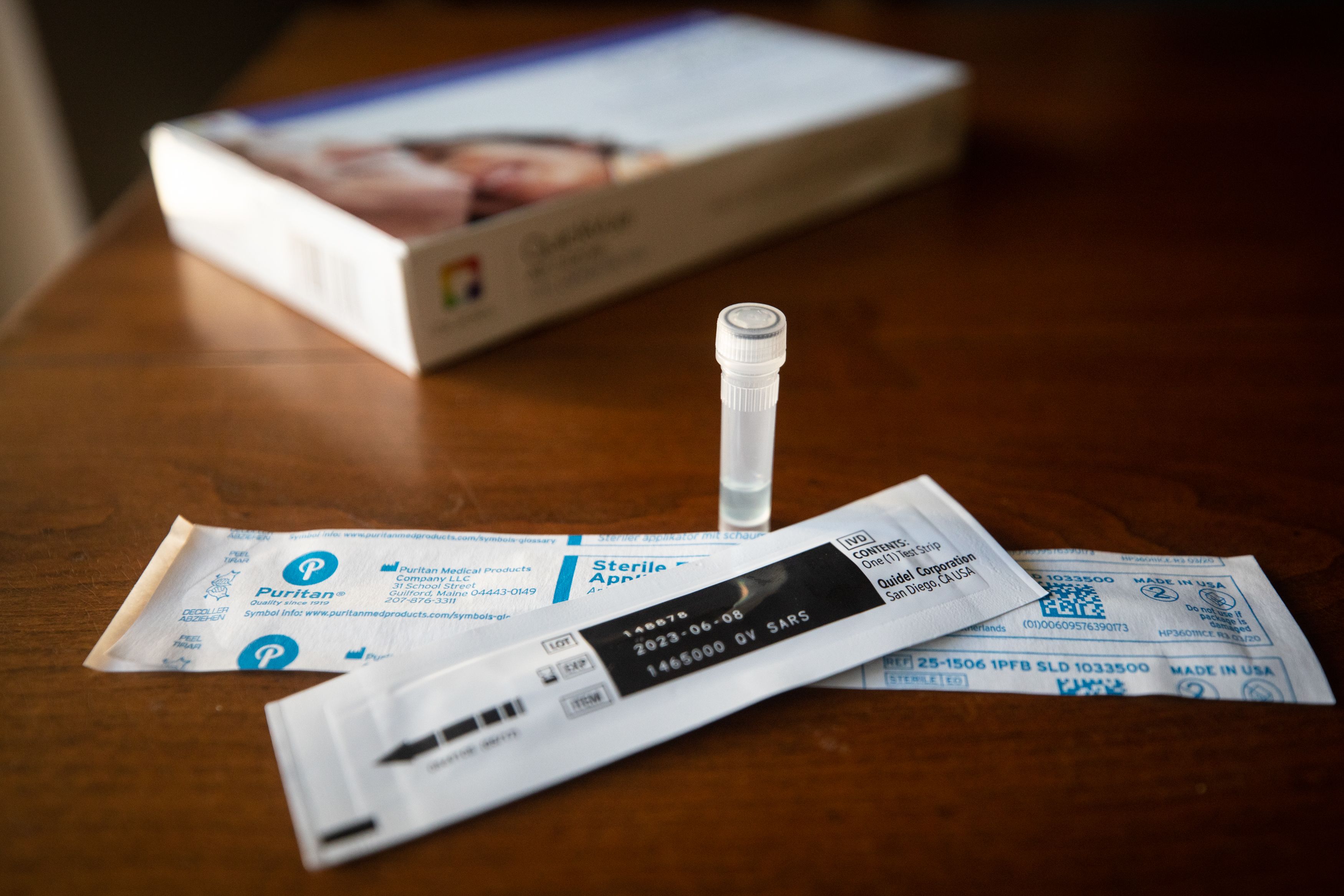
Gabriel C. Pérez / KUT
Gabriel C. Pérez / KUT
Dr. Verduzco-Gutierrez, prevention is obviously the best way to avoid COVID. But what would you suggest for people who think they might be experiencing symptoms of long COVID: What should they do, and how should they recognize it?
MV: When someone has had COVID and they may be experiencing some of the symptoms, I definitely recommend that get to their health care professional. Hopefully more and more healthcare professionals are getting educated on it. We've written a set of consensus guidance statements for many of the most common symptoms related to long COVID that are available for all health care providers.
And so they should seek and get help. We don't have a cure yet, but there are at least treatments that can help some of the major symptoms related to long COVID.
Credits
"The State of Disability in Texas" was reported and produced by Michael Marks,
Alexandra Hart, Sarah Asch, Glorie Martinez, Molly-Jo Tilton
and Shelly Brisbin.
Managing editor Gabrielle Muñoz, digital producer Raul Alonzo,
and social media editor Wells Dunbar put together the digital presentation.
Our visuals editor was Deborah Cannon.
Managing producer Laura Rice was our editor and showrunner.
Texas Standard's director is Leah Scarpelli. Our technical director
is Casey Cheek.
Our host for this special was Shelly Brisbin, who also provided editorial
oversight.
The music for "The State of Disability in Texas" was curated by
Leah Scarpelli and features artists and musicians who are part of
the organization the Recording Artists Music Professionals
with Disabilities (RAMPD):